Table of Contents:
While this subject is shrouded in mystery and misconceptions, owing to societal taboos and lack of accessible information, vaginal laxity is encountered by many women all over the world. Vaginal laxity can have significant repercussions on a woman’s physical comfort, sexual satisfaction, and overall quality of life. Despite its magnitude and menace, many women feel isolated or embarrassed to seek help, often enduring the symptoms in silence.

Whether you’re experiencing vaginal laxity yourself or seeking to support someone who is, this comprehensive guide helps understand its causes, recognize its symptoms, and explore the diverse treatment options available.
What Is Vaginal Laxity?
Vaginal laxity refers to the stretching or loosening of the vaginal walls, resulting in reduced tightness. According to the International Continence Society and the International Urogynecological Association, it is simply defined as an excessive looseness of the vaginal tissue.

Research shows that a significant portion (28–40%) of women seeking treatment at urogynecology clinics experience vaginal laxity to a degree that affects their overall well-being.
What Causes Vaginal Laxity?
Vaginal laxity can arise from a variety of factors, often interconnected and complex. Below are the common factors that result in loosening of the vagina.
1. Vaginal Delivery
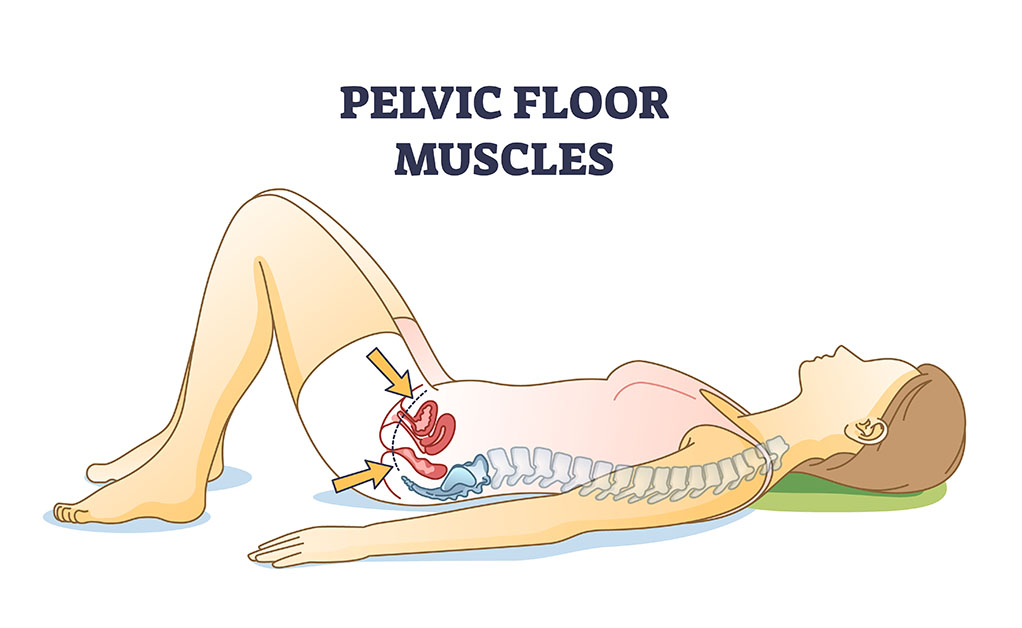
While there are multiple ways to tighten the vagina after childbirth, this is the most common cause of vaginal laxity. During delivery, the vaginal walls, pelvic floor muscles, and connective tissues undergo significant stretching to allow for the passage of the baby. The extent of this stretching can vary depending on several factors:
Parity: Women who have had multiple vaginal deliveries (high parity) are more likely to experience vaginal laxity due to repeated stretching and potential tissue damage.
Size of the Baby: Delivering a larger baby can cause more stretching and extensive tearing of the vaginal tissues.
Instrumental Deliveries: The use of forceps or vacuum during delivery can also contribute to increased trauma and subsequent laxity.
Episiotomy and Tears: Surgical cuts (episiotomies) or perineal tears that occur during delivery can weaken the vaginal and perineal muscles, causing some laxity.
2. Ageing
As women age, their body undergoes natural changes that affect the elasticity and strength of tissues. The decline in elastin and collagen fibres as well as the declining estrogen levels leads to thinning, drying, and reduced elasticity of the vaginal walls. These age-related changes contribute to vaginal laxity.
3. Hormonal Changes
Hormonal fluctuations throughout a woman’s life, particularly during pregnancy, breastfeeding, and menopause, significantly impact the structural integrity of the vaginal walls and pelvic floor muscles.
4. Pregnancy
Elevated levels of estrogen and relaxin during pregnancy soften and relax pelvic tissues to accommodate childbirth.
5. Breastfeeding
During breastfeeding, elevated prolactin levels suppress estrogen production, resulting in vaginal tissues becoming thinner, less elastic, and more susceptible to dryness and atrophy. This decrease in estrogen leads to reduced collagen production and impaired tissue repair, causing increased laxity in the vaginal area.
6. Menopause
A significant decline in estrogen levels during menopause leads to vaginal atrophy, characterized by thinning, drying, and reduced elasticity of the vaginal walls.
7. Genetic Factors
Genetic predisposition can influence the strength and resilience of connective tissues. Women with a family history of pelvic floor disorders may be more likely to experience vaginal laxity due to inherited traits that affect tissue elasticity.
8. Lifestyle Factors
Obesity: Excess body weight puts additional pressure on the pelvic floor muscles, leading to their weakening over time.
Smoking: Smoking affects blood flow and tissue health, reducing the ability of tissues to repair and maintain themselves, thereby causing vaginal laxity.
Chronic Straining: Activities that involve repeated straining, such as heavy lifting, chronic coughing, or constipation, can weaken the pelvic floor muscles.
9. Connective Tissue Disorders
Certain medical conditions that affect connective tissues, such as Ehlers-Danlos syndrome, can predispose women to pelvic floor dysfunctions, including vaginal laxity.
What Are The Symptoms Of Vaginal Laxity?

The symptoms of vaginal laxity include:
- A feeling of looseness in the vaginal area
- A reduced sensation during sexual intercourse
- Decreased sexual satisfaction
- Difficulty in reaching orgasm
- If you are still menstruating, you might notice that tampons tend to slip out.
- Urinary incontinence or leakage. In severe cases fecal incontinence.
- If left untreated, pelvic organ prolapse may develop.
How Can A Diagnosis Of Vaginal Laxity Be Made?

Diagnosing vaginal laxity is typically clinical and involves a combination of medical history, physical examination, and sometimes additional diagnostic tests. Below are the steps typically involved in diagnosing vaginal laxity:
1. Medical History
The healthcare provider will begin by taking a detailed medical history, which may include:
Symptoms: Discuss any symptoms you may be experiencing, such as decreased vaginal tightness, urinary incontinence, or discomfort.
Childbirth History: Inquiring about the number of vaginal deliveries, any complications during childbirth, the birth weight of the baby/babies, and whether instrumental deliveries were involved.
Menstrual and Reproductive History: Including information about pregnancies, breastfeeding, and menopause status.
Lifestyle Factors: Inquiring about factors such as smoking, obesity, and chronic constipation, which can contribute to pelvic floor dysfunction.
Questionnaires: Patient-reported outcome measures or questionnaires may be used to assess symptoms related to vaginal laxity and pelvic floor dysfunction.
2. Physical Examination
A thorough physical examination will be conducted, which may involve:
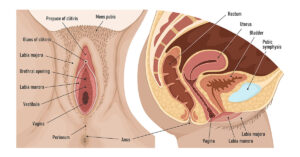
Pelvic Examination: The healthcare provider will examine the external and internal structures of the vagina and pelvic floor. They may assess the tone and strength of the pelvic floor muscles and evaluate the integrity of the vaginal walls.
Q-Tip Test: In some cases, a Q-tip test may be performed to assess vaginal laxity. This involves gently inserting a Q-tip into the vaginal canal and evaluating the degree of tightness or looseness felt around the Q-tip.
3. Additional Tests
Depending on the findings from the medical history and physical examination, additional tests may be recommended:
Pelvic Ultrasound: An ultrasound scan may be used to visualize the pelvic organs and assess any structural abnormalities or prolapse.
Pelvic Floor Muscle Assessment: Some healthcare providers may conduct specialized tests, such as electromyography (EMG) or pelvic floor dynamometry, to measure muscle strength and function.
If you suspect you have vaginal laxity or are experiencing related symptoms, it is essential to consult with a healthcare provider specializing in women’s health and pelvic floor disorders for an accurate diagnosis and personalized treatment plan tailored to your specific needs.
Preventive Measures Against Vaginal Laxity

Preventive measures against vaginal laxity encompass a range of lifestyle practices and proactive strategies aimed at maintaining the strength and elasticity of the vaginal tissues and pelvic floor muscles.
1. Pelvic Floor Exercises
Regularly practising pelvic floor exercises can significantly strengthen the pelvic floor muscles. These exercises involve contracting and relaxing the muscles that support the pelvic organs, improving muscle tone and enhancing the ability to control bladder and bowel functions.
2. Maintain a Healthy Weight
Maintaining a healthy body weight through a balanced diet and regular exercise helps reduce excess pressure on the pelvic floor muscles. Excess weight can strain these muscles, weakening them over time.
3. Avoid Heavy Lifting and Straining
Avoiding activities that increase intra-abdominal pressure, such as lifting heavy objects improperly or straining during bowel movements, can help prevent unnecessary stress on pelvic floor muscles and connective tissues.
4. Manage Chronic Conditions
Managing chronic conditions that can contribute to pelvic floor dysfunction, such as chronic coughing (e.g., from smoking or respiratory conditions) and constipation, is crucial. Addressing these conditions through medical treatment and lifestyle modifications can help prevent further strain on the pelvic floor muscles.
5. Healthy Lifestyle Choices
Making healthy lifestyle choices, such as avoiding smoking and excessive alcohol consumption, can promote overall tissue health and support pelvic floor function.
Treatment Options for Vaginal Laxity
There are several treatment options available for the management of this condition.
1. Pelvic Floor Exercises and Physical Therapy
Pelvic floor exercises, such as Kegel exercises, aim to strengthen the pelvic floor muscles, thereby improving muscle tone and supporting the vaginal walls. The benefits include improved muscle tone, enhanced vaginal support, reduced symptoms of urinary incontinence, and enhanced sexual satisfaction.
2. Non-Surgical Treatments
a. Laser Therapy
Mechanism of Action: Laser vaginal rejuvenation treatments use fractional CO2 or erbium lasers to induce controlled thermal damage to the vaginal tissues. This stimulates collagen production and improves tissue elasticity.
Description: During the procedure, the laser energy penetrates the vaginal walls, triggering a healing response that enhances blood flow, thickens the vaginal mucosa, and tightens the vaginal canal.
Benefits: Increased vaginal tightness, improved lubrication, enhanced tissue elasticity, and alleviation of mild urinary incontinence symptoms.
b. Radiofrequency (RF) Therapy
Mechanism of Action: Radiofrequency vaginal rejuvenation treatments deliver thermal energy to the vaginal tissues, stimulating collagen production and remodelling of the vaginal mucosa.
Description: RF energy heats the deeper layers of the vaginal tissues, promoting tightening and rejuvenation. This non-invasive treatment encourages tissue contraction and improves vaginal tone over a series of sessions.
Benefits: Enhanced vaginal tightness, improved urinary continence, increased blood circulation to the vaginal area, and minimal discomfort or downtime as opposed to surgical treatment.
3. Surgical Interventions
a. Vaginoplasty
Mechanism of Action: Vaginoplasty is a surgical procedure that aims to tighten the vaginal canal by removing excess vaginal lining and repairing stretched or weakened muscles.
Description: During vaginoplasty, the surgeon removes redundant vaginal tissue and tightens the underlying muscles to restore vaginal tightness and support.
Benefits: Significant improvement in vaginal tightness and sexual satisfaction, correction of structural abnormalities, and long-lasting results.
b. Perineoplasty
Mechanism of Action: Perineoplasty focuses on repairing and reconstructing the tissues of the perineum, which is the area between the vagina and anus. This improves overall vaginal support and tightness.
Description: The procedure involves trimming excess perineal skin, repairing episiotomy scars, and reinforcing the perineal muscles to enhance vaginal tone and function.
Benefits: Improved perineal appearance, enhanced vaginal support, reduced laxity, and improved sexual sensation.
4. Hormonal Therapy
Mechanism of Action: Hormone replacement therapy (HRT) or localized estrogen treatments aim to replenish declining estrogen levels, which play a crucial role in maintaining vaginal tissue health and elasticity.
Description: HRT involves the administration of estrogen, either orally, through patches, or vaginal creams, to restore vaginal moisture, thickness, and elasticity. Localized estrogen treatments are applied directly to the vaginal tissues to alleviate symptoms of vaginal atrophy and improve tissue integrity.
Benefits: Increased vaginal lubrication, enhanced tissue elasticity, reduced discomfort during intercourse, and overall improvement in vaginal health.
The choice of treatment for vaginal laxity depends on various factors, including the severity of symptoms, individual health considerations, and personal preferences.
The Importance Of Professional Assistance
It is essential to understand and address vaginal laxity for women’s health and well-being. This condition can significantly impact the quality of life, affecting physical comfort, sexual satisfaction, and pelvic health.

Consulting with a specialist in urogynecology or pelvic floor disorders is crucial to assess your specific needs and goals. At Labiaplasty NYC, we recommend tailored treatment plans that address our patients’ concerns effectively and improve their overall pelvic health and quality of life. By understanding the mechanisms and benefits of each treatment option, women can make informed decisions to manage vaginal laxity and regain confidence in their pelvic health.
References
- Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourology and Urodynamics: Official Journal of the International Continence Society. 2010 Jan;29(1):4-20.
- Campbell P, Krychman M, Gray T, Vickers H, Money-Taylor J, Li W, Radley S. Self-reported vaginal laxity—prevalence, impact, and associated symptoms in women attending a urogynecology clinic. The Journal of Sexual medicine. 2018 Nov;15(11):1515-7.
- Dietz HP, Stankiewicz M, Atan IK, Ferreira CW, Socha M. Vaginal laxity: what does this symptom mean?. International urogynecology journal. 2018 May;29:723-8.
- Aulia I, Valeria M. Current Perspectives in Vaginal Laxity Measurement: A Scoping Review. Arch Plast Surg. 2023 Aug 31;50(5):452-462. doi: 10.1055/a-2113-3202. PMID: 37808327; PMCID: PMC10556325.