Menopause is a natural biological ageing process that marks the end of a woman’s menstrual cycle and reproductive years1. It also marks the near cessation of hormonal activity by the ovaries.
Natural menopause is defined as the permanent end of menstrual cycles, confirmed after 12 consecutive menses-free months without identifiable physiological or pathological cause, and without medical or surgical interventions such as radiotherapy, certain chemotherapy or surgical removal of the ovaries1.
Most women typically experience menopause between the ages of 45 and 55 years, with an average of 51 years. This has been the same since antiquity; however, because life expectancy is increasing, women now spend almost one-third of their lives in the postmenopausal phase2.
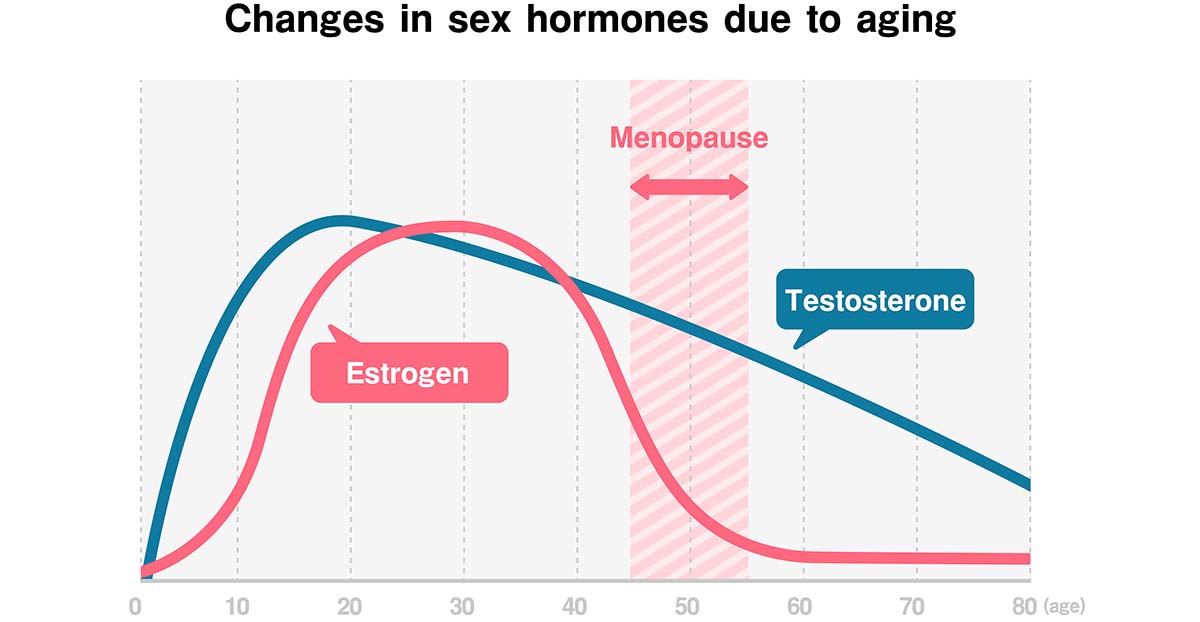
Because menopausal transition is driven by a gradual decline in ovarian function and key reproductive hormones, the age ranges for menopause vary significantly. When menopause occurs before 40 years of age, it is known as premature menopause; when it occurs between 40 and 45 years, it is early menopause, and after 55 years, it is known as late menopause.
Menopause and sex are closely linked. The period not only affects physical health, relationships, and self-esteem but also causes noticeable changes in sexual health, leading to symptoms such as vaginal dryness in menopause, discomfort during intimacy, and reduced libido. Despite this, many women believe it’s something they must silently endure, but awareness and evidence-based support can make all the difference.
Understanding Menopause and Hormonal Shifts
As menopause approaches, levels of hormones released by the aging ovaries, such as estradiol, progesterone, anti-Müllerian hormone (AMH) and inhibin B, begin to decline. The reduction in ovarian hormones reduces negative feedback, thereby increasing the levels of follicle-stimulating hormone (FSH) produced by the pituitary gland. The fall of estradiol, inhibin B and AMH and the rise of FSH mark the end of the reproductive years3.

There is also a decline in testosterone, a hormone that influences both metabolism and menopause and sex, which can contribute to how menopause affects libido and sexual function.
Impacts of Hormonal Changes on the Body
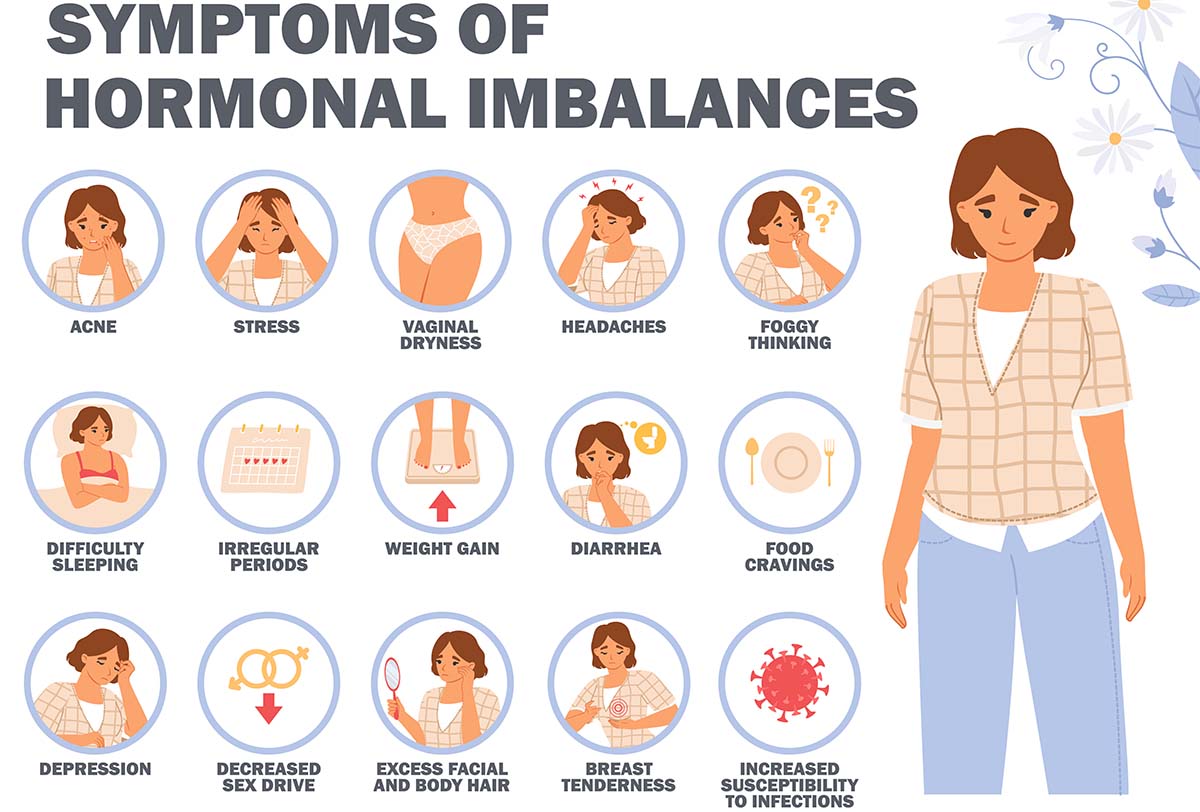
The declining hormones, particularly estrogen, progesterone, and to a lesser extent testosterone, have wide-ranging effects on the menopausal woman, some of which include;
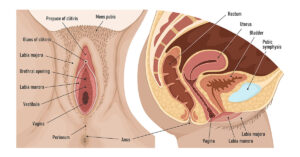
1. Bladder and Pelvic Floor Changes
- Decreasing estrogen levels can increase the risk of urinary tract infections and can weaken the pelvic floor support, leading to lower urinary tract dysfunction, with some women having urinary urgency, incontinence and even pelvic organ prolapse.
2. Bones and Joints
- Because estrogen plays a role in maintaining bone density, its decline leads to bone loss, thereby increasing the risk of fractures. Some women also complain of joint pain and stiffness, which can be attributed to the effects of low estrogen and ageing.
3. Cardiovascular System
- Estrogen’s protective effect on the heart and blood vessels helps to keep arteries flexible and cholesterol levels balanced. Hence, after menopause, women face a higher risk of cardiovascular disease, including hypertension and the buildup of plaque in stiffening blood vessels.
4. Metabolism and Weight
- The changes in hormone levels can slow down metabolism and lead to fat accumulation, especially around the abdomen. It can also increase the risk of type 2 diabetes and metabolic syndrome due to insulin resistance.
- Some women have also reported increased appetite or cravings during the menopausal period, which can inadvertently lead to weight gain.
5. Skin, Hair, and Body Composition
- Skin elasticity, its collagen and moisture retention are all supported by estrogen; hence, low hormone levels lead to thinner, less elastic and drier skin. The diminishing estrogen levels are also implicated in hair thinning and loss
- Over time, there may be a loss of muscle mass and an increase in fat mass.
6. Mood, Brain, and Sleep
- During the menopausal transition, irritability, anxiety, and depression may be reported. This is partly due to estrogen’s role in modulating neurotransmitters like serotonin and dopamine6.
- Lapses in memory, difficulty concentrating (often called “brain fog”), and insomnia can affect emotional and mental health.
7. Vasomotor System
Vasomotor symptoms, which are hypothalamically mediated, are by far the most widely reported symptom of menopause (affecting 80% of women)4. They are characterized by a sudden sensation of heat with flushing of the skin, discomfort, palpitations, and sweating. These feelings often last several minutes but are some of the more temporary symptoms and usually resolve with time.
Common Menopause Effects on Sex: What’s Normal
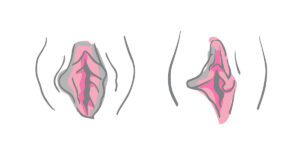
1. Genital Changes
- Reduced production of estrogen by the ovaries causes vaginal wall thinning, decreased vaginal wall elasticity and reduced production of fluids and mucus that keep the vagina lubricated and supple. This can lead to vaginal itching, dryness, burning sensation and even discomfort or painful sex during menopause.
- The wall of the vagina may become more fragile, and the vaginal canal may become shorter over time (vaginal atrophy), leading to menopause and intimacy issues.
- Together with the urinary symptoms associated with menopause, these symptoms are now known as genitourinary syndrome of menopause.
2. Decreased Libido
Some women report a reduction in sexual desire during and post menopause, which may be due to the combined effects of low estrogen, fatigue, body image concerns and changes in relationship dynamics, explaining how menopause affects libido.
3. Longer Time to Arousal
With hormonal changes and sex drive in menopause, it is normal for arousal to take longer and for genital response, such as swelling and lubrication, to be less pronounced or slower. These changes can affect spontaneous sexual activity and may require more stimulation to become fully aroused.
4. Changes in Orgasm
Some will have a harder time reaching orgasm or find that their orgasms are no longer as intense. This may be due to reduced blood supply and nerve sensitivity at the genitals, as well as due to psychological factors like mood disturbances and anxiety.
What’s Not Normal: Signs That Warrant Medical Attention
While many sexual changes during menopause are expected, some symptoms go beyond what is typical and require medical evaluation. These could signal conditions beyond menopause effects on sex and should not be ignored. Recognizing these red flags is essential to ensure that treatable issues are not overlooked or dismissed.
1. Persistent or Severe Pain During Intercourse (Dyspareunia)
Occasional discomfort and slight pain may be normal, but intensely painful sex during menopause is not and may be due to infections or other pelvic disorders that require treatment.
2. Bleeding After Intercourse
Postcoital bleeding is not a typical symptom of menopause and should always be evaluated. It may be as a result of vaginal atrophy or something more serious, like precancerous or cancerous changes in the cervix or uterus.
3. Sudden Loss of Sexual Desire
A gradual decline in libido can be expected, but a sudden drop or severe loss in sexual interest may be a result of depression or other psychological conditions.
4. Urinary Incontinence
A significant percentage of menopausal women experience urinary incontinence; however, this may worsen over time if left unaddressed.
If you’re experiencing any of these issues, remember that you don’t have to simply “put up with it.” Effective solutions are available when you seek help from your healthcare providers.
How Medical Treatments and Experts Can Help
A wide range of menopause sexual health treatments and professional support are available to help women regain comfort, confidence, and intimacy.
Here’s how advanced medical treatments can assist:
1. Hormone Replacement Therapy (HRT)
HRT involves supplementing the body’s depleting hormones with synthetic estrogen (sometimes combined with progesterone) to relieve symptoms like vaginal dryness during menopause, vaginal atrophy, hot flushes, and mood disturbances. Although there is still debate concerning its benefit-risk ratio, localized estrogen therapy (such as vaginal creams, rings, or tablets) which specifically target genital symptoms usually has only minimal to no systemic side effects.
2. Non-Hormonal Treatments
For those in whom hormone therapy is contraindicated or who just prefer not to use it, non-hormonal options like vaginal lubricants can help improve vaginal comfort and reduce pain during intercourse. For vasomotor symptoms, certain medications such as paroxetine and fezolinetant, approved by the FDA, diminish these symptoms and result in improved quality of life.
3. Pelvic Floor Therapy
Pelvic floor physical therapy strengthens the muscles that support the bladder, uterus, and rectum. It is used to manage incontinence, pelvic pain, and decreased sexual sensation. Techniques like Kegel exercises and biofeedback are commonly used and help enhance menopause and intimacy outcomes.
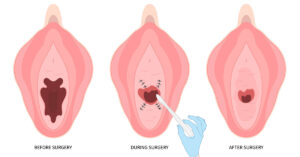
4. Vaginal Rejuvenation Treatments
Vaginal rejuvenation refers to a variety of surgical and non-surgical treatments designed to restore the structure, feel and function of the vaginal and vulvar tissues. In menopausal women, they are particularly useful for vaginal dryness, laxity, discomfort during intercourse, reduced sexual sensation, urinary incontinence, and to improve the cosmetic appearance of the labia.
The following are several types of Vaginal Rejuvenation Treatments that may be beneficial;
1. Radiofrequency Therapy (e.g., ThermiVa)
ThermiVa uses controlled radiofrequency energy to gently heat the vaginal tissues, thereby stimulating collagen and elastin production5. This helps to enhance sensation, improve vaginal lubrication and tighten the canal. It also strengthens the tissues around the urethra, improving mild to moderate urinary incontinence.
2. Laser Therapy (e.g., MonaLisa Touch, FemTouch)
Here, fractional CO? (like FemiLift) or Er: YAG lasers deliver micro-injuries to the vaginal wall, prompting the tissue to heal itself by generating new collagen, blood vessels, and epithelial cells5. This improves vaginal tone, thickness, and lubrication and is ideal for less severe degrees of urinary incontinence. Treatments are typically done in 2-3 or more sessions, each lasting a few minutes, with only minimal discomfort.
3. O-shot injections
This involves drawing out the client’s own blood to concentrate the thrombocytes and re-injecting it into specific areas of the vaginal and clitoral tissues. The goal is to promote tissue repair, increase sensitivity, and improve sexual satisfaction.
4. Vaginoplasty
This is a vaginal tightening surgery that tightens the vaginal canal by restoring muscular and fascial support, often through dissection and suturing of the underlying tissues. This can improve sexual intimacy, quality of life and overall menopause effects on sex.
5. Counseling for Sexual Health
Sex therapists, psychologists, and psychiatrists can help address issues like low libido, anxiety, depression, or challenges in relationships. Therapy provides a safe space to express problems, frustrations, and discover strategies to cope and improve confidence.
The Do’s & Don’ts During Menopause
Navigating menopause can be a challenging time for many women. While hormonal changes can affect sexual health and overall well-being, adopting certain practices can help manage these changes and improve quality of life.
Here’s a guide to the dos and don’ts during this period:
Do:
1. Communicate with Your Partner
- Open communication with your partner about menopause and sex, changes in your body, mood and intimacy is an important step in maintaining a fulfilling relationship.
2. Seek Professional Help if Needed
- Never hesitate to consult a healthcare provider about menopause sexual health if you are unsure of what’s happening to you or if you experience unexpected symptoms.
3. Use Vaginal Moisturizers or Lubricants
- Over-the-counter water-based lubricants or vaginal moisturizers help combat vaginal dryness in menopause, making sex more comfortable.
4. Maintain a Healthy Lifestyle
- Engaging in regular exercise, eating a balanced diet, and having good sleep can improve your mood, energy levels, and overall health. Kegel exercises strengthen the pelvic muscles and help manage urinary incontinence or pelvic prolapse.
5. Try Vaginal Rejuvenation Treatments
- Symptoms of genitourinary syndrome of menopause (GSM), such as vaginal dryness, laxity, or discomfort during intercourse, may improve with non-surgical treatments like radiofrequency therapy or laser therapy.
6. Address Emotional Health
- Aging is a blessing, so be easy on yourself. If you’re feeling anxious, depressed, or disconnected, seek counseling or therapy.
Don’ts:
1. Don’t Ignore Pain
- If you’re experiencing sexual changes during menopause like persistent genital pain or a burning sensation, don’t ignore it. Seek medical attention.
2. Don’t Feel Ashamed or Embarrassed
- Menopause and sexual health changes are a natural part of life. Don’t be embarrassed to talk about your symptoms with your doctor, partner, or a specialist.
3. Don’t Ignore Mental and Emotional Changes
- Hormonal fluctuations can lead to mood swings, anxiety, or depression. Don’t neglect these feelings; seek professional support.
4. Don’t Stop Contraception Too Early
- During the perimenopausal period, there might be a slight risk of pregnancy until the levels of Follicle Stimulating Hormone reach the postmenopausal range. If you don’t wish to become pregnant, contraception is still recommended until at least 12 months after your last period.
5. Don’t Avoid Sex Completely
- It’s common for libido to decrease during menopause, but completely avoiding sex due to discomfort or emotional factors can affect intimacy and sexual function. If possible, try to address the underlying issues using over-the-counter treatments, seeking professional help and communicating with your partner.
6. Don’t Engage in Risky Sexual Practices
- Even when pregnancy is no longer a concern, it’s still important to protect yourself from sexually transmitted infections (STIs). Use condoms if you have multiple partners or if you or your partner has not been tested for STIs.
FAQs on Menopause & Related Conditions
1. How long do the sexual symptoms of menopause last?
The duration of sexual symptoms varies widely among women. Some symptoms, like vaginal dryness, reduced libido or painful sex during menopause, may persist for years or even worsen over time if not treated. Others may improve with treatment or lifestyle changes.
2. What’s the difference between perimenopause and menopause?
Perimenopause is the transitional phase leading up to menopause. It is marked by fluctuating hormone levels and irregular periods. It can begin in the early or late 40s and last for several years. Menopause, on the other hand, is confirmed when a woman has gone 12 consecutive months without her menstrual period.
3. Is it possible to get pregnant during perimenopause and menopause?
Though fertility declines during perimenopause, pregnancy is still possible until menopause is fully reached. Once a woman has attained menopause, natural conception is no longer possible except through artificial reproductive techniques (In vitro Fertilization with donor eggs).
4. Should I still see a gynecologist after menopause?
Yes. Postmenopausal women still benefit from regular gynecological visits to monitor pelvic health and screen for conditions like cervical cancer.
5. How long should post-menopausal women use HRT?
Postmenopausal women can use hormone replacement therapy (HRT) for symptom relief, usually for 3–5 years, but longer use may be appropriate if symptoms persist or for osteoporosis prevention. The decision should be individualized, with regular reviews by your healthcare provider to ensure benefits outweigh risks. Guidelines recommend using the lowest effective dose and continuing HRT as long as it’s needed and safe.
6. What is the advice for menopause occurring in younger women?
For younger women with early or premature menopause (before age 40), HRT is recommended until the average age of natural menopause (around 51) to protect against bone loss, heart disease, and other long-term health risks.
7. How should unscheduled bleeding in menopausal women on HRT be managed?
Menopausal women on HRT who have unscheduled bleeding should be assessed based on HRT type and duration. While common in the first 3–6 months, persistent or new bleeding after this period requires evaluation, including pelvic exam, ultrasound, and possibly endometrial biopsy to rule out serious causes.
Reclaiming Comfort and Confidence After Menopause
While menopause is a natural transition, the physical and sexual changes it brings can affect quality of life. Symptoms like hot flushes and vaginal dryness are common and treatable. With the right information and support, women can maintain comfort, confidence, and intimacy well into their postmenopausal years.
At our advanced vaginal rejuvenation clinic in NYC, we offer expert gynecological advice and personalized treatments, including non-surgical and surgical solutions, to help you feel like yourself again. If you’re struggling with intimacy, dryness, or discomfort, contact us today to schedule a confidential consultation and explore options tailored to your needs.
References
- World Health Organization. Menopause. 2024. Accessed July 15, 2025. https://www.who.int/news-room/fact-sheets/detail/menopause#:~:text=Most%20women%20experience%20menopause%20between,changes%20in%20the%20menstrual%20cycle.
- Statistics CNCfH. Life Expectancy. U.S. Department of Health & Human Services. 2024. Accessed November 16, 2024. https://www.cdc.gov/nchs/fastats/life-expectancy.htm
- De Vet A, Laven JS, de Jong FH, et al. Antimüllerian hormone serum levels: a putative marker for ovarian aging. Fertil Steril. 2002;77(2):357–362. DOI: 10.1016/S0015-0282(01)02993-4
- Avis NE, Crawford SL, Greendale G, et al. Duration of Menopausal Vasomotor Symptoms Over the Menopause Transition. JAMA Intern Med. 2015;175(4):531–539. doi:10.1001/jamainternmed.2014.8063
- Salvatore S, Nappi RE, Zerbinati N, et al. “A 12-week treatment with fractional CO? laser for vulvovaginal atrophy: a pilot study.” Climacteric. 2015;18(1):125–132. https://doi.org/10.3109/13697137.2014.971454
- Soares CN. “Depression and menopause: current knowledge and clinical recommendations for a critical window.” Psychiatr Clin North Am. 2014 Jun;37(2):259–274. https://doi.org/10.1016/j.psc.2014.02.001