Vaginal atrophy is a progressive, estrogen-deficiency-related condition that affects millions of women globally. Yet, it remains widely underdiagnosed and undertreated. Beyond just vaginal dryness, vaginal atrophy symptoms include structural tissue changes, pain, urinary dysfunction, and even clitoral atrophy.
This article presents a comprehensive overview of vaginal atrophy, including its causes, symptoms and evidence-backed treatment for vaginal atrophy, and answers to the most common patient FAQs. It also highlights integrative and regenerative options like topical vaginal estrogen, the O-Shot, vaginal fat transfer and fillers to support optimal vulvovaginal health.
What Is Vaginal Atrophy?
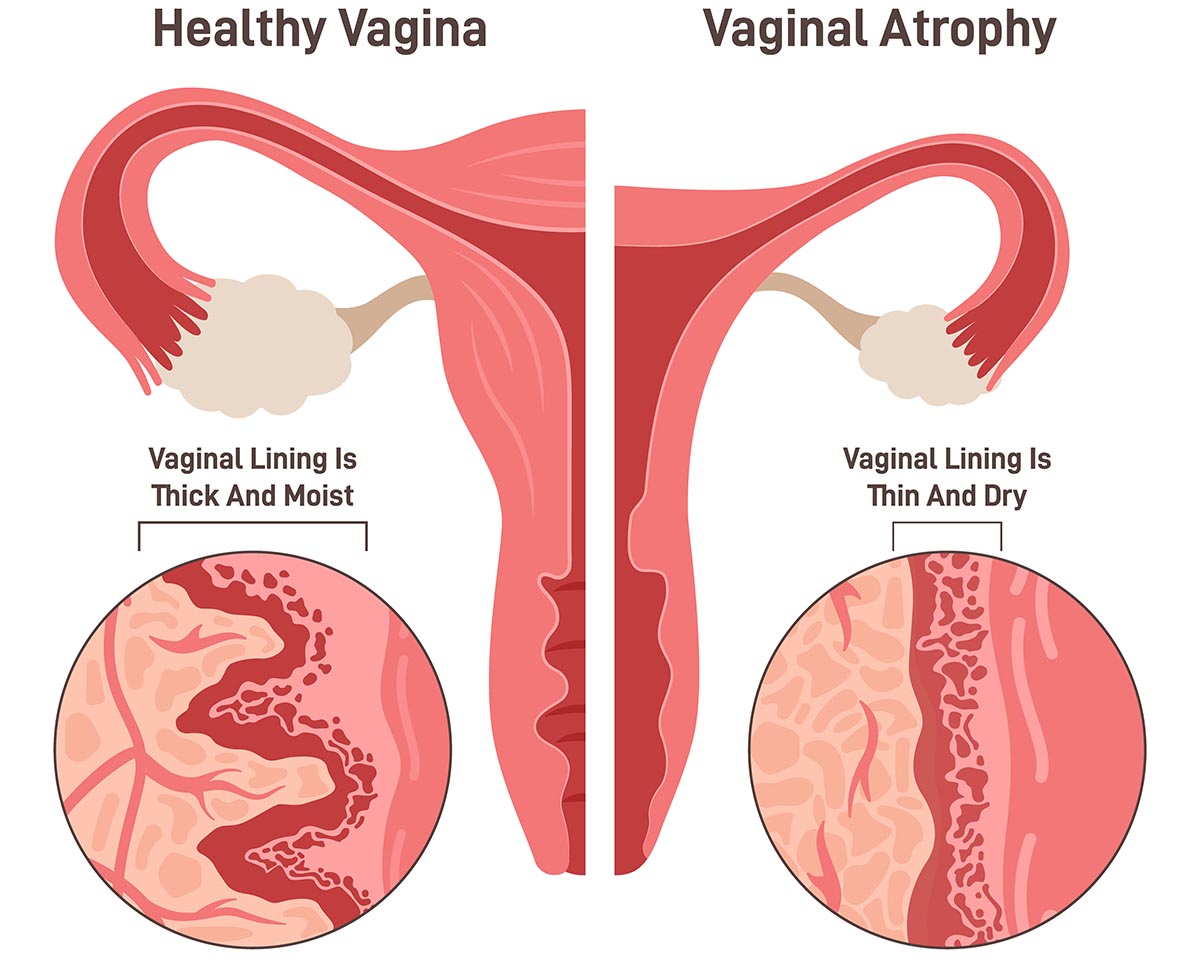
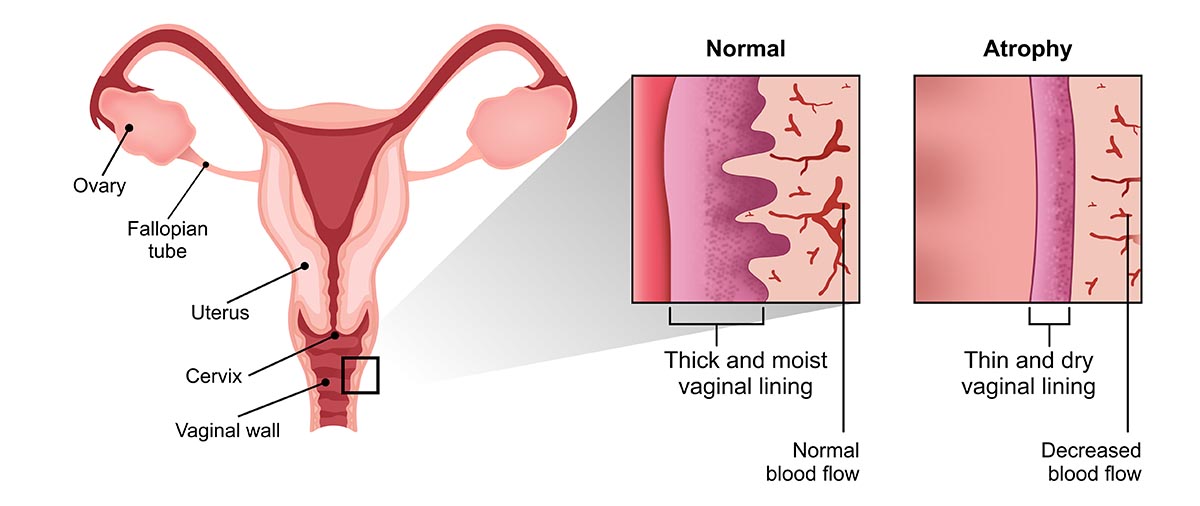
Vaginal atrophy refers to the thinning, drying, and loss of elasticity of the vaginal walls due to a significant decline in estrogen levels. This condition primarily affects postmenopausal women, but can also occur in:
- Breast cancer survivors
- Women undergoing chemotherapy, radiation, or oophorectomy
- Those using anti-estrogen therapies (e.g., aromatase inhibitors)
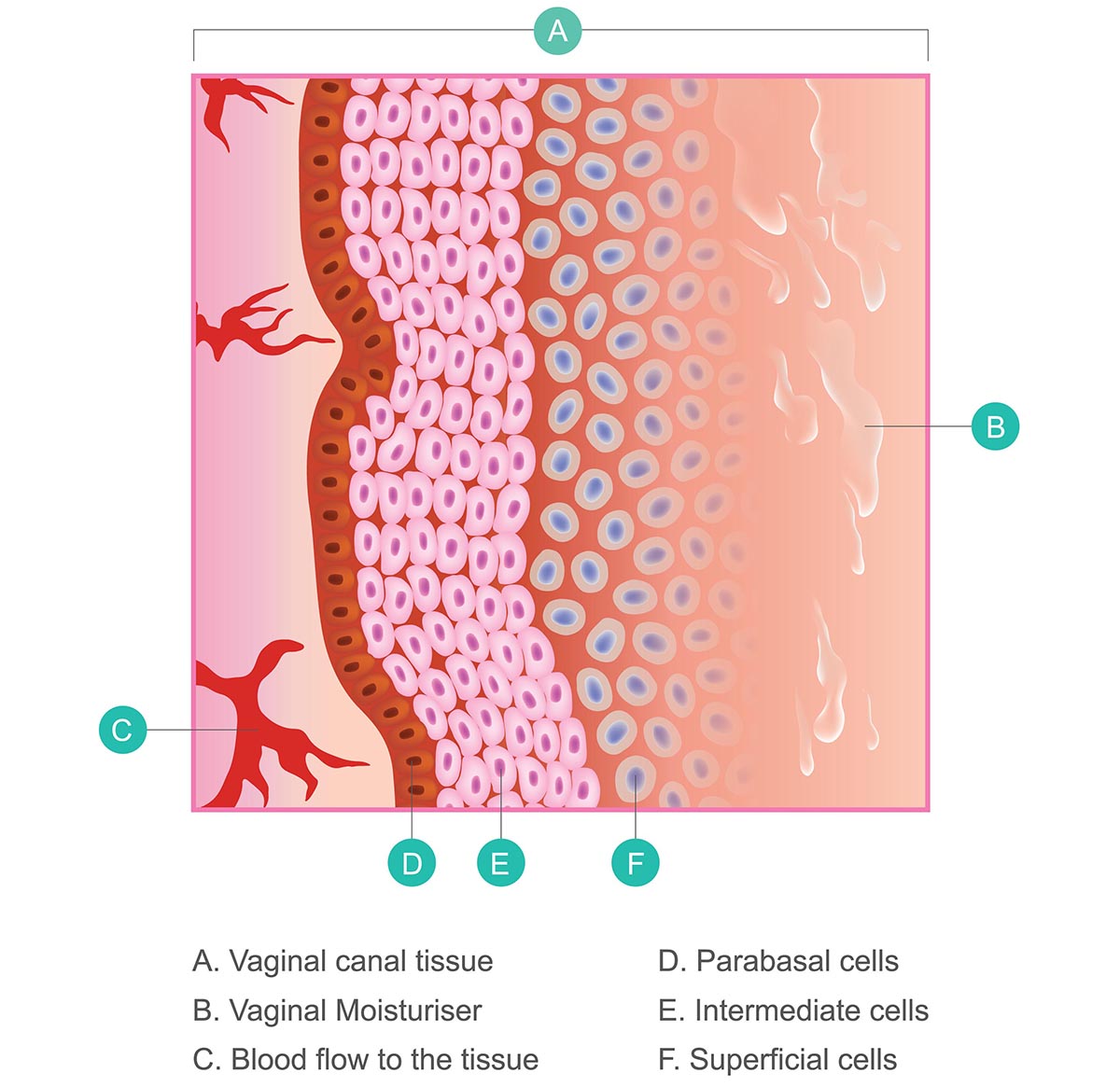
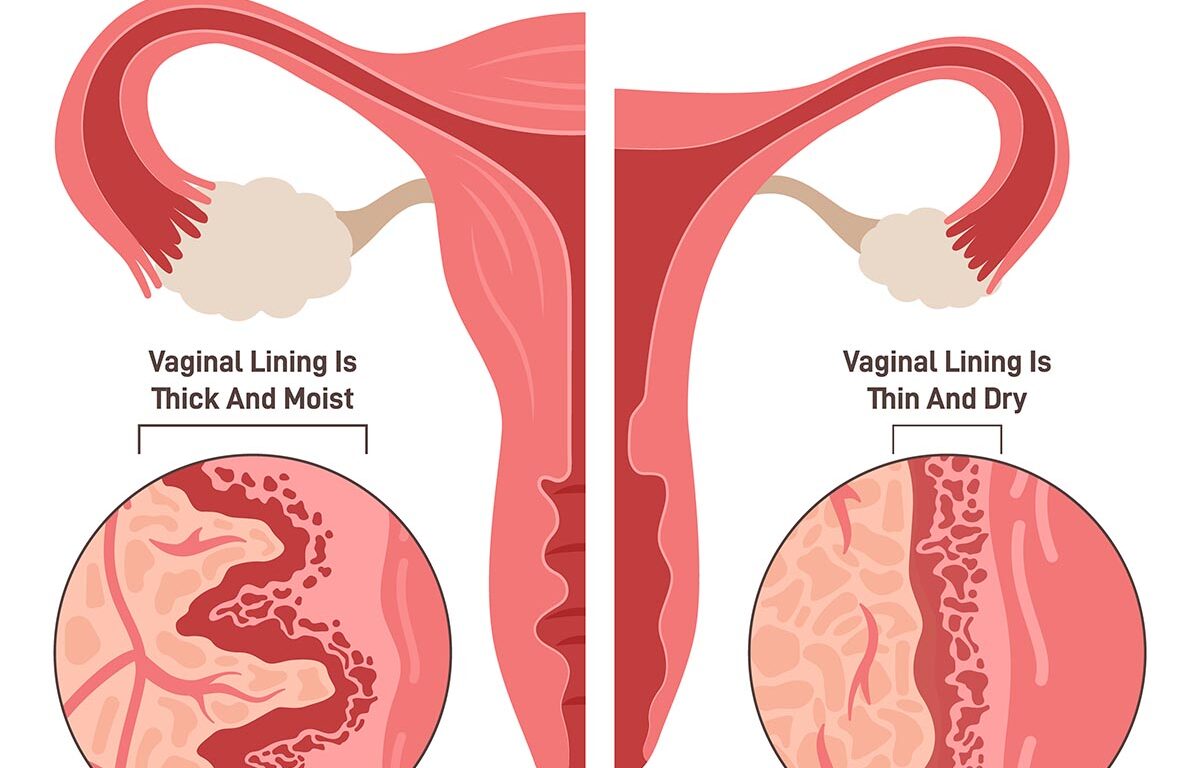
Estrogen plays a vital role in maintaining the vaginal epithelium’s thickness, vascularity, and microbiome. When estrogen levels drop, the vaginal tissue becomes fragile, less lubricated, and more prone to microtears, inflammation, and discomfort.
What Causes Vaginal Atrophy?
As discussed, vaginal atrophy causes are linked to estrogen deficiency. This can occur naturally during menopause, or prematurely due to surgery, cancer treatment, or anti-estrogen medications. Estrogen is key for maintaining vaginal microbiome, pH, and tissue resilience1.
The predominant vaginal atrophy causes include:
- Natural menopause (typically between ages 45–55)
- Premature or surgical menopause
- Postpartum estrogen suppression (especially during lactation)
- Certain medications: Tamoxifen, GnRH analogs, aromatase inhibitors
- Radiation or chemotherapy affecting the pelvic region
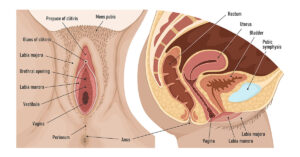
Estrogen receptors are present throughout the vulvovaginal tissue, urethra, and bladder, making this a multisystem condition, not just a gynecologic one1.
Vaginal Atrophy Symptoms
Vaginal atrophy symptoms can range from mild to debilitating and often mimic other conditions like infections or lichen sclerosus. Common symptoms include:
- Vaginal dryness, burning, or itching
- Dyspareunia (painful intercourse)
- Vaginal tightness or shortening
- Spotting or bleeding after sex
- Decreased arousal or lubrication
- Clitoral atrophy or reduced clitoral sensitivity
- Recurrent UTIs and urinary urgency/frequency
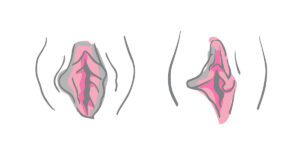
In advanced cases, visible loss of labial volume or thinning of the labia majora may be observed due to estrogen-related fat and collagen depletion.
Diagnosis and Assessment
Diagnosis is primarily clinical. A thorough history and pelvic examination are essential. Findings may include:
- Pale, smooth vaginal mucosa
- Loss of rugae
- Elevated vaginal pH (>5)
- Thinned labia or clitoral atrophy
- Fragility or pinpoint bleeding
When symptoms are ambiguous, consider ruling out infection, lichen planus, or neoplasia via cultures or biopsy.
How to Treat Vaginal Atrophy

There are multiple ways to treat this condition depending on severity, medical history, and patient preferences. These include:
- Daily topical vaginal estrogen
- Non-hormonal moisturizers
- Biostimulation (e.g., O-Shot)
- Vaginal laser or radiofrequency
- Counseling for sexual health
- Use of vaginal dilators (especially in cases of stenosis)
Before undergoing energy-based or surgical treatments, it is essential to understand what to ask your cosmetic gynecologist before a procedure, from safety and downtime to long-term outcomes.
Evidence-Based Vaginal Atrophy Treatment Options
1. Topical Vaginal Estrogen Therapy (First-Line)
Topical estrogen is the gold standard for vaginal atrophy treatment, offering localized symptom relief without significant systemic absorption2. Options include:
- Estradiol cream
- Vaginal tablets
- Estrogen-releasing vaginal ring
Most women notice improvement within 2–4 weeks.
2. Non-Hormonal Therapies
For women who cannot take estrogen (e.g., breast cancer survivors), non-hormonal options are critical:
- Regular vaginal moisturizers (2–3x/week)
- Use water or silicone-based lubricants before intercourse
- Hyaluronic acid-based vaginal gels
These options relieve symptoms but do not reverse the underlying atrophy.
3. Regenerative & Integrative Therapies
Emerging modalities for treating vaginal atrophy include:
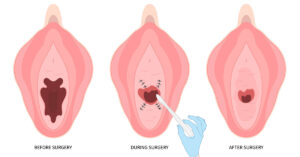
- O-Shot: Stimulates collagen production and improves mucosal hydration
- Laser therapies (CO2 or Er: YAG): Promote epithelial renewal
- Vaginal Fat Transfer and Fillers: Restore lost volume in the labia majora and vestibular region, particularly in cases of clitoral atrophy
- Use of designer vagina procedures with labial augmentation or resurfacing, when appropriate
These interventions are promising but should be performed by skilled providers in women’s health or cosmetic gynecology.
Non-Hormonal Innovations: Core Intima (CO? Laser) and O-Shot
Two of the most effective non-surgical, non-hormonal treatments for vaginal atrophy are Core Intima and the O-Shot. These advanced modalities use either laser energy or regenerative growth factors to restore tissue health, moisture, and function.
1. Core Intima (CO? Laser Therapy)
Core Intima is a fractional CO? laser specifically designed for the treatment of vaginal atrophy and vaginal rejuvenation.
How It Works:
- Delivers controlled microablative energy to the vaginal epithelium
- Stimulates collagen synthesis, neovascularization, and mucosal thickening
- Enhances hydration, elasticity, and pH normalization
Benefits:
- Improves vaginal tightness and lubrication
- Reduces dryness, burning, and dyspareunia
- Requires no anesthesia or downtime
- Usually administered as a series of 3 sessions
Best for:
- Postmenopausal women
- Breast cancer survivors (who require non-hormonal solutions)
- Women with mild urinary incontinence or vaginal laxity
2. O-Shot (Orgasm Shot Using Growth Factors)
The O-Shot involves injecting growth factors, derived from the patient’s own blood, into the anterior vaginal wall and clitoral area.
How It Works:
- The bioactive growth factors promote nerve and tissue regeneration
- Improves vascularity, mucosal health, and sensation
Benefits:
- Enhances vaginal lubrication and elasticity
- Reduces pain during intercourse
- Improves orgasmic response and sexual satisfaction
- May reduce stress urinary incontinence
Treatment Overview:
- Performed in-office in about 30 minutes
- Involves drawing and spinning the patient’s own blood to isolate the growth factors
- No downtime or anesthesia required
What Does Vaginal Atrophy Look Like?
The visual indicators for vaginal atrophy include:
- Thinned, pale vaginal lining
- Loss of rugae (vaginal folds)
- Labial fusion or clitoral atrophy
- Stenosis or shortened vaginal canal
- Loss of labial plumpness (often prompting use of Vaginal Fat Transfer and Fillers)
How to Prevent Vaginal Atrophy
While vaginal atrophy is a natural consequence of declining estrogen, especially during menopause, there are proactive steps you can take to delay its onset, reduce symptom severity, and maintain long-term vaginal health.
- Maintain regular sexual activity or use vaginal dilators to preserve elasticity
- Start topical estrogen therapy early in menopause, if appropriate
- Avoid douching and irritants
- Use non-hormonal moisturizers proactively
- Manage chronic conditions (e.g., diabetes, autoimmune disorders)
Preventive care is especially important for women undergoing medically induced menopause or cancer treatment.
Can You Reverse Vaginal Atrophy?
When diagnosed early, vaginal atrophy is largely reversible with appropriate care:
- Topical vaginal estrogen thickens the epithelium and restores function within weeks
- Laser and regenerative therapies offer additional support
- Combining medical and lifestyle interventions produces the best outcomes3
Consistent, long-term treatment is essential, as symptoms often return when therapy is discontinued.
Restoring Vaginal Health with Advanced Care
Vaginal atrophy is a progressive, under-recognized condition with far-reaching effects on quality of life, intimacy, and urinary health. Fortunately, with the right mix of evidence-based and regenerative interventions, women can reclaim vaginal function and comfort.

Whether you are in early menopause or struggling with persistent vaginal atrophy symptoms, don’t wait. Speak to a women’s health expert or cosmetic gynecologist about your options, including topical estrogen, non-hormonal alternatives, and other advanced therapies.
At our state-of-the-art vaginal rejuvenation clinic in NYC, we offer expert-led, evidence-based treatments, including the O-Shot, laser therapies, and vaginal fat transfer and fillers to help you restore comfort, function, and confidence. Book your confidential consultation today and take the first step toward lasting relief.
References
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy. Menopause. 2014;21(10):1063-1068. doi:10.1097/GME.0000000000000329
- Kingsberg SA, Wysocki S, Borgeat A, Constantine G. Vulvar and vaginal atrophy in postmenopausal women: prevention and treatment. Mayo Clin Proc. 2017;92(4):649-660. doi:10.1016/j.mayocp.2017.02.016
- Archer DF, Labrie F, Grondin L, et al. A review of clinical experience with local estrogen therapy for the treatment of vaginal atrophy. Clin Interv Aging. 2022;17:47-58. doi:10.2147/CIA.S343419