Table of Contents:
- Introduction
- Brief overview of the concept of virginity and its cultural significance
- What is Hymenoplasty?
- Common Reasons Why Women Opt For the Procedure (cultural, personal, or psychological reasons)
- The Hymenoplasty Procedure
- Recovery Process and Aftercare
- Immediate Post-Operative Recovery
- First Week of Recovery
- Two to Four Weeks Post-Operative
- Long-Term Care and Monitoring
- FAQs About Hymenoplasty
- Conclusion
The concept of restoring virginity holds personal, religious, cultural, and emotional importance. Whether it’s for religious beliefs, cultural traditions, or personal healing, the choice to reclaim virginity can be deeply meaningful. Hymenoplasty has emerged as a popular option for women who seek to regain this symbolic state, helping them restore a sense of wholeness and control over their bodies.
While the decision to have a hymenoplasty is a personal one, knowing what the procedure involves is important. From the first consultation to the recovery period, it’s crucial to be well-informed and comfortable throughout the process. Many women who choose hymenoplasty find that it offers more than just physical restoration; it can also help boost confidence and bring a sense of emotional healing and empowerment.
Brief overview of the concept of virginity and its cultural significance
Virginity, often understood as a lack of experience with sexual intercourse, has held significant cultural, religious, and social importance across various societies for centuries. 1,2 Traditionally, it has been seen as a marker of purity, particularly for women, and is closely tied to ideas of morality, honour, and virtue.3 In many cultures, virginity is valued as an essential quality before marriage, symbolizing innocence and fidelity, often shaping gender expectations and social roles.2

In some communities, an intact hymen holds significant socio-cultural value as “proof” of a woman’s virginity, leading to the practice of “virginity testing.” This involves a vaginal examination to assess whether a woman’s hymen is “intact,” or the expectation of bloodstains after first intercourse, stemming from the belief that the hymen “breaks” and bleeds upon initial sexual experience.4,5 In reality, examination to check whether the hymen is intact is not a reliable indicator of sexual history, as this tissue can be stretched or torn due to various non-sexual activities like sports, and there are natural anatomical differences that mimic a “torn hymen”.6 Furthermore, the expectation of bloodstains is misleading as this only occurs when the hymen is thicker and less pliable; hence, not all women bleed during their first sexual encounter.6
Medical experts are increasingly challenging these practices, and in 2018, the World Health Organization (WHO) officially called for an end to virginity testing.1
What is Hymenoplasty?
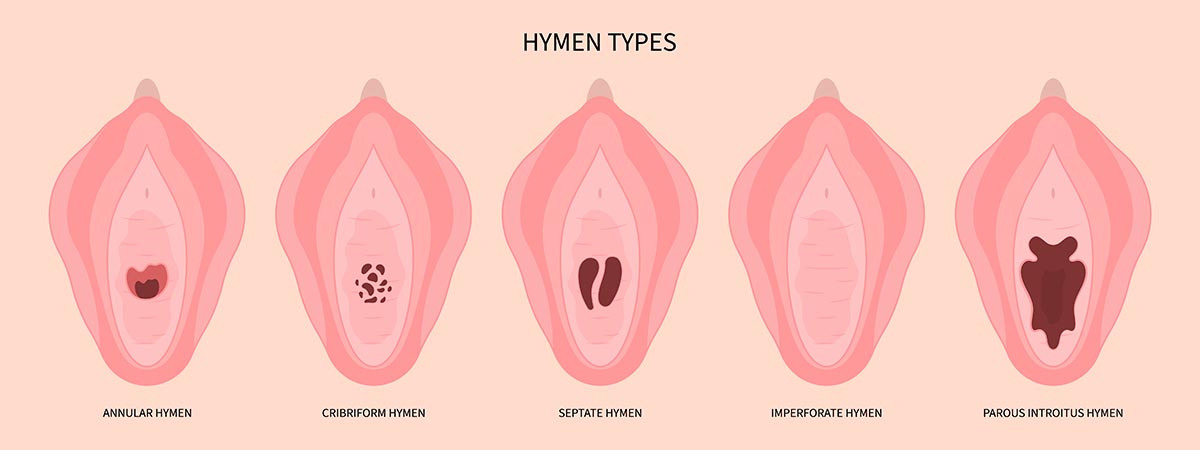
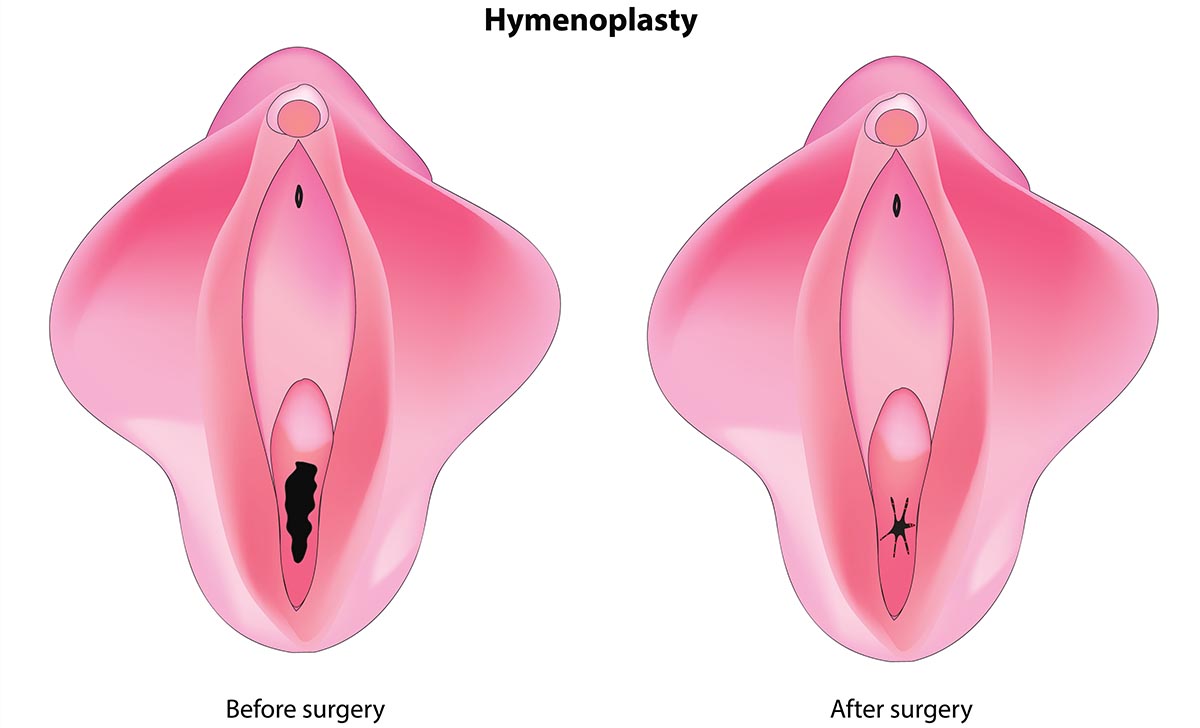
The hymen itself is a thin layer of tissue that forms during early development and sits just behind the vaginal opening. Its shape and thickness vary from person to person.6
Hymenoplasty is a surgical procedure that repairs or reconstructs the hymen.7 While the procedure is often performed for cosmetic or cultural reasons, it offers no direct medical benefit. Instead, hymenoplasty caters to personal or societal expectations surrounding virginity.8 The reconstructed hymen will function similarly to a natural hymen. It may tear and bleed during intercourse or remain intact, depending on the tightness and structure created during the surgery. With the right care, most women can expect full recovery within 6 to 8 weeks, with no complications.
Common Reasons Why Women Opt For the Procedure (cultural, personal, or psychological reasons)
Hymenoplasty is chosen by women for various reasons. Here are some of the key motivations:
1. Cultural and Religious Pressures
In many societies, virginity is highly valued, particularly before marriage. Women may undergo hymenoplasty to meet cultural or religious expectations and avoid stigma or judgment from families or communities.
2. Personal Choice and Control
Some women choose hymenoplasty to reclaim control over their bodies or past experiences. This decision can help them feel a sense of renewal, especially after regretful or forced sexual experiences.
3. Psychological Well-Being
Hymenoplasty can provide peace of mind and reduce anxiety about relationships, particularly for women concerned about societal pressures or future partners’ expectations regarding virginity.
Overall, hymenoplasty offers emotional and psychological relief for women facing societal pressures, personal insecurities, or the need to heal from past trauma.
The Hymenoplasty Procedure
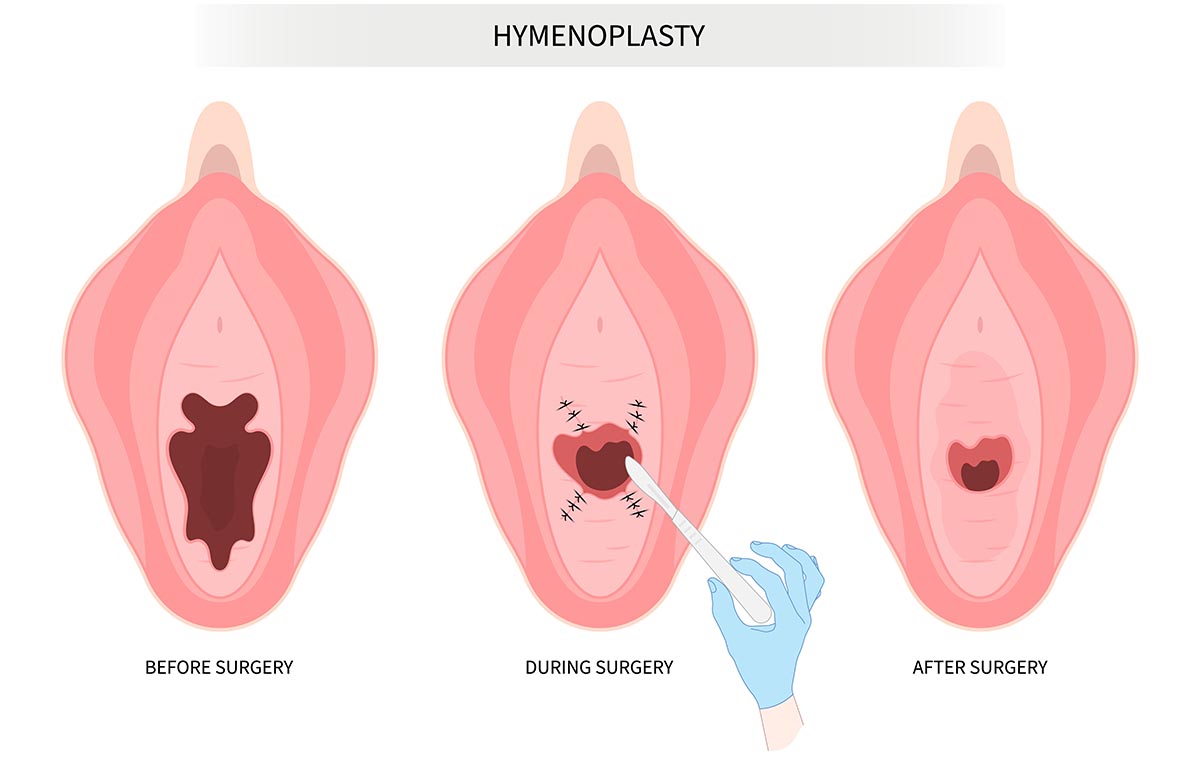
Hymenoplasty is a straightforward outpatient surgical procedure that lasts 30 minutes – 1 hour. It is performed to reconstruct or restore the hymen.
1. Patient Positioning and Preparation
The patient is placed in the lithotomy position, where the patient lies on her back with her legs elevated and supported by stirrups. This position provides optimal access for the surgeon to perform the procedure.
The vaginal area is thoroughly cleansed using an antiseptic solution to reduce the risk of infection, and sterile drapes are placed around the surgical field to maintain a clean surgical field.
2. Anesthesia
In most cases, a local anesthetic agent like lidocaine is applied, which numbs the vaginal area and surrounding tissues around the hymen while the patient remains awake. If necessary or preferred, general or regional anesthesia may be administered. Under general anesthesia, the patient is unconscious throughout the procedure.
3. Reconstruction Process
If sufficient hymenal tissue is available, the surgeon carefully pulls the remnants of the hymen together. These fragments are brought close to each other to recreate a continuous membrane. The surgeon uses fine, absorbable sutures to stitch the tissue together. These sutures will dissolve over time, allowing the hymen to heal naturally.
The newly formed hymen is left with a small central opening, similar to a natural hymen. This opening is crucial for maintaining the appearance and function of a typical hymen and the egress of menstrual blood flow.
In cases where there are no sufficient hymenal remnants, the surgeon may need to create a new hymen using tissue from the vaginal lining. A small flap of the inner vaginal wall is carefully cut and shaped into a hymen-like structure.
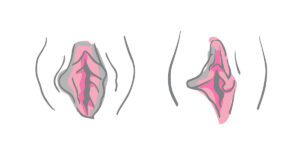
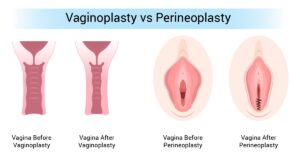
4. Tightening of the Vaginal Opening (Optional)
Perineoplasty: In some cases, women may also request a slight tightening of the vaginal opening along with the hymenoplasty procedure. This is achieved by suturing the vaginal entrance in a way that narrows it, which can enhance the sensation of tightness during intercourse. Other optional services include vaginoplasty and labiaplasty
Recovery Process and Aftercare
Hymenoplasty is a relatively minor surgical procedure, and most women experience a straightforward recovery. However, following proper aftercare guidelines is essential for healing, comfort, and minimizing the risks of complications. Below is a detailed guide to the recovery process and aftercare after hymenoplasty.
Immediate Post-Operative Recovery
1. Post-Surgery Monitoring
- After the procedure, patients are monitored in a recovery area for a short time to ensure they are stable, especially if general anesthesia was used. Once the anesthesia wears off and there are no immediate complications, patients are discharged, typically within a few hours.
2. Initial Sensations and Discomfort
- It’s common to experience mild pain, discomfort, or tightness in the vaginal area immediately after the procedure. Most women describe the sensation as moderate soreness, similar to menstrual cramps or after strenuous physical activity.
- Swelling and slight bruising around the vaginal area may also occur, but generally subsides within a few days.
- Vaginal discharge or spotting is normal during the initial days post-surgery. Light bleeding or pinkish discharge may last up to a week.
3. Pain Management
- Painkillers: Over-the-counter pain medications like ibuprofen or acetaminophen are usually prescribed to alleviate discomfort. Your surgeon may prescribe stronger pain relief depending on the level of discomfort.
- Cold Compresses: Using cold packs on the outer vaginal area (wrapped in a cloth to prevent direct contact with the skin) can help reduce swelling and relieve pain in the first 24 to 48 hours post-surgery.
First Week of Recovery

1. Rest and Avoiding Strain
- Rest is crucial during the first few days after hymenoplasty. Patients should avoid strenuous activities such as lifting heavy objects, intense exercise, or any physical strain, as it could disrupt the healing process.
- Gentle walking is encouraged to promote blood circulation, but any activity that involves the pelvic muscles should be minimized.
2. Personal Hygiene and Care
- Keeping the Area Clean: Hygiene is key to preventing infection. The external genital area should be cleaned gently with water and mild, unscented soap. After washing, the area should be patted dry, not rubbed.
- Avoid Baths: For the first two weeks, avoid soaking in a bath, swimming pool, or hot tub. These activities can introduce bacteria into the vaginal area and increase the risk of infection. Stick to showers and avoid direct water pressure on the surgical site.
- Wound Care: The stitches used are dissolvable, so there is no need to remove them. However, avoid touching or interfering with the area unnecessarily, as it can cause irritation or disrupt the healing process.
Two to Four Weeks Post-Operative

1. Resuming Normal Activities
- After the first week, patients can typically return to light daily activities, such as walking or gentle household tasks. However, strenuous activities and exercise should still be avoided for at least four weeks. Avoid using tampons until the area has fully healed, typically around 6- 8 weeks. The use of tampons can disrupt healing or cause infections.
- It’s important to follow the surgeon’s specific timeline regarding when certain activities can be resumed, as individual healing rates may vary.
2. Wearing Loose Clothing
- Tight clothing, such as skinny jeans or restrictive underwear, can cause friction and irritation in the healing area. Opt for loose-fitting underwear and breathable, cotton-based clothing to ensure comfort and prevent irritation.
Long-Term Care and Monitoring
1. Follow-Up Appointments
- Patients are usually scheduled for a follow-up appointment with their surgeon about 1 to 2 weeks after the surgery to assess the healing process. During this visit, the surgeon will check for any signs of infection and address any concerns the patient may have.
- Additional follow-up appointments may be necessary depending on the healing progress and any complications that arise.
2. Signs of Complications
While most hymenoplasty procedures heal without issues, it’s important to monitor for signs of complications. Contact your healthcare provider if you notice:
- Increased pain or swelling that worsens after the first few days.
- Heavy bleeding or discharge with a foul odour, which could be a sign of infection.
- Fever or chills, which could also indicate an infection.
- Difficulty urinating or excessive pain during urination.
3. Healing Timeline
- Complete healing of the hymenoplasty typically occurs within 6 to 8 weeks. At this point, the hymen will have fully healed, and any residual tenderness or discomfort should subside.
FAQs About Hymenoplasty
1. Is hymenoplasty painful?
The surgery itself is not painful, as it is performed under anesthesia (local, regional or general). After the procedure, mild to moderate discomfort or soreness in the vaginal area is common, but this can be managed with over-the-counter pain medications. Most discomfort subsides within a few days.
2. Will the hymen be completely restored?
Hymenoplasty reconstructs the hymen to a state that mimics its original form. The hymen will appear intact, and in some cases, it may tear and bleed during subsequent intercourse. However, the extent to which the reconstructed hymen functions like a natural one depends on individual anatomy and the surgical technique used.
3. Can hymenoplasty be detected?
In most cases, hymenoplasty is difficult to detect through a standard gynecological exam, as the reconstruction mimics the natural hymen. However, highly trained specialists may be able to detect the surgery. Typically, it is a procedure with results that are not distinguishable by most observers.
4. Does hymenoplasty affect fertility or future pregnancies?
No, hymenoplasty does not affect a woman’s fertility or her ability to become pregnant in the future. The procedure only reconstructs the hymen at the vaginal opening and does not interfere with reproductive organs such as the uterus, ovaries, or fallopian tubes.
5. How long do the results of hymenoplasty last?
The results of hymenoplasty are permanent until the hymen is torn, usually during intercourse or physical activities that affect the vaginal area. Once the hymen tears, it will not regenerate naturally.
6. Can hymenoplasty be combined with other procedures?
Yes, hymenoplasty can be combined with other vaginal cosmetic or reconstructive surgeries, such as labiaplasty, perineoplasty or vaginoplasty, depending on the patient’s goals. It’s important to discuss all desired procedures with your surgeon during the consultation.
7. Is hymenoplasty covered by insurance?
In most cases, hymenoplasty is considered a cosmetic procedure and is not covered by health insurance. However, the cost may vary depending on the clinic, surgeon, and location.
Professional Care For Vaginal Rejuvenation Procedures
Hymenoplasty is a personal and culturally sensitive procedure that offers women the option to reconstruct their hymen for various reasons, whether due to cultural expectations, personal healing, or emotional closure.
While the surgery itself is relatively quick and involves a straightforward recovery process, it’s important to understand the potential risks and limitations. Hymenoplasty does not affect fertility or long-term health but requires careful aftercare for optimal healing. Reclaim your confidence with Alinea Labiaplasty NYC‘s expert hymenoplasty services. Contact us today to learn more.
References
- Lillis JK. Virginity in healthcare. InPalgrave Encyclopedia of the Health Humanities 2023 Jan 31 (pp. 1-6). Cham: Springer International Publishing.
- Olson RM, García-Moreno C. Virginity testing: a systematic review. Reprod Health. 2017;14(1):61
- Bhana D. Virginity and virtue: African masculinities and femininities in the making of teenage sexual cultures. Sexualities. 2016;19(4):465–481.
- Independent Forensic Expert Group. Statement on virginity testing. J Forensic Legal Med. 2015a;33:121–4.
- Olson RM, García-Moreno C. Virginity testing: a systematic review. Reprod Health. 2017;14:61.
- Hymenoplasty. [ Jun; 2023 ]. 2023. https://www.gov.uk/government/publications/expert-panel-on-hymenoplasty/hymenoplasty-background-paper. https://www.gov.uk/government/publications/expert-panel-on-hymenoplasty/hymenoplasty-background-paper.
- Sissa G. The hymen is still a problem. Virginity, imperforation, and contraception, from Greece to Rome. EuGeStA. 2013;3:67–123.
- Christianson M, Eriksson C. Myths and misconceptions: midwives’ perception of the vaginal opening or hymen and virginity. Br J Midwifery. 2013;21(2):108–115