Table of Contents:
- Overview
- What to Expect During Vaginoplasty Recovery
- Immediate Post-Operative Care
- The First Week of Recovery Following a Vaginoplasty
- The First Month: Gradual Healing After a Vaginoplasty
- Long-Term Recovery: Months Two to Six After a Vaginoplasty
- Potential Complications Following a Vaginoplasty and How to Handle Them
- When to Seek Medical Attention
- Proper Recovery With Professional Care
- References
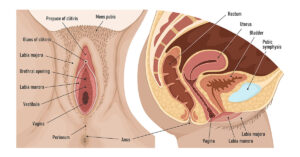
Vaginoplasty is a surgical procedure designed to enhance or restore the vaginal area, offering solutions to a variety of concerns that individuals may face due to ageing, childbirth or other factors. Vaginoplasty has become an increasingly sought-after procedure, not only for its physical benefits but also for its profound impact on a person’s confidence and overall well-being.

Earlier, vaginoplasty and related vaginal tightening procedures were primarily performed to repair damage resulting from childbirth. These procedures aimed to restore the vaginal area’s function and support after obstetrical delivery.1
In recent years, however, the scope of vaginoplasty has broadened significantly. It is now increasingly sought after also for its potential to address sexual and aesthetic concerns, reflecting a more comprehensive understanding of its benefits beyond post-delivery repair.2 Today, vaginoplasty is often categorized under cosmetic surgeries marketed as “vaginal rejuvenation” or “designer vagina” procedures.
What to Expect During Vaginoplasty Recovery
The success of vaginoplasty relies not only on the surgical technique but also on the patient’s commitment to a well-structured recovery plan. Recovery, as with any surgery, is a gradual process, with each stage requiring attention to postoperative care instructions to ensure the best possible results.

Recovering from vaginoplasty surgery involves several stages, each with specific care requirements and expectations. Understanding what to anticipate can help ensure a smoother recovery process and optimize the procedure’s final results.
Immediate Post-Operative Care
1. Initial Assessment
Right after your surgery, you will be transported to the recovery room. This specialized area provides immediate care as you recover from anesthesia. Here, medical staff will continuously monitor your vital signs to ensure your safety as the effects of anesthesia wear off. These vitals include your heart rate, blood pressure, temperature, respiratory rate and oxygen levels. Any significant deviations will be addressed promptly.
2. Effects of Anesthesia
As you recover from anesthesia, you might feel groggy, disoriented, or experience mild nausea. These effects are typically temporary and will diminish as the anesthetic wears off. Staff will be attentive to any adverse effects from the anesthesia, and additional medications may be given, if necessary, to manage these symptoms.
3. Pain Management
Effective pain management is crucial to ensure a comfortable recovery after a vaginoplasty. Medical staff will frequently assess your pain levels using a standardized pain scale, and you will be encouraged to communicate openly about your pain levels. Pain management will include the use of oral or injectable non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen and/or opioids.
4. Wound Care
Immediately after your vaginoplasty, a sterile dressing may be applied to the surgical site. This dressing serves important functions of surgical site protection and absorption of discharge and bleeding. This dressing may be changed during recovery if it becomes soaked.
The First Week of Recovery Following a Vaginoplasty

After a vaginoplasty, the first week is a critical period in your recovery process. This time is essential for your body to begin healing from the surgery and for you to adapt to the vaginoplasty side effects and postoperative care requirements. Here’s a detailed guide on what to expect and how to manage your initial vaginoplasty recovery time:
1. Pain and Swelling
Pain: Some pain or discomfort can be expected at this time. However, you will likely be prescribed pain medications to help with this. In addition to medications, applying a cold pack wrapped in a cloth to the area can help reduce swelling and provide additional pain relief. Avoid placing ice directly on the skin to prevent frostbite.
Swelling: Swelling and bruising are common post-surgery and typically peak within the first few days. Elevate your legs when possible and avoid activities that could worsen the swelling.
2. Reduced Mobility and Activity
Some limitations in movement may be expected, but light movement is encouraged to improve blood circulation, which aids in healing and reduces the risk of blood clots. You will, however, be advised to avoid activities that can put a strain on the surgical site, such as penetrative sex and jogging, to allow your body to heal.
3. Wound Care
Maintain hygiene to prevent infection. Use a mild, non-scented soap with lukewarm water to clean the area. A squirt bottle may be beneficial. Gently pat the area dry with a clean towel. Antibiotics may also be prescribed to prevent wound infection. You will need to continue monitoring the surgical site for signs of infection, such as increased redness or swelling, warmth, or unusual discharge and report any concerns to your healthcare provider immediately.
4. Emotional and Psychological Well-being
Recovery can be emotionally challenging. You might experience a range of emotions, from anxiety about the healing process to frustration with limitations on your activity. Lean on friends, family, or a counsellor if needed. Emotional support is crucial during recovery to help manage stress and anxiety.
5. Follow-Up Care
You will be expected to attend all follow-up appointments as scheduled. These visits are essential for your surgeon to assess your healing progress, address any complications, and provide guidance on resuming normal activities. Use these appointments to ask any questions you may have about your recovery. Discuss any issues you are experiencing, whether physical or emotional.
The First Month: Gradual Healing After a Vaginoplasty

The first month following a vaginoplasty is a pivotal period where you transition from the initial recovery phase to more active healing and rehabilitation. This time is crucial for establishing a solid foundation for your long-term recovery and adapting to the changes post-surgery. Here’s what you can expect and how to manage your recovery during this critical period:
1. Healing Progress
Reduction in Swelling: Swelling and bruising that were prominent in the first week should gradually decrease. Before the end of the month, you should notice a resolution of these symptoms.
Change in Pain Levels: Pain and discomfort diminish early on. You may still experience occasional soreness, but it should be less intense compared to the first week. Adjustments in pain medication may be necessary, and your healthcare provider will guide you on transitioning to over-the-counter options if appropriate.
Wound Maturation: During the first month, the surgical site’s initial healing progresses as the tissues continue to repair. This period involves the formation of new tissue and the strengthening of the surgical site.
2. Resuming Normal Activities
Light Exercise: During this period, you can begin incorporating light exercises as your surgeon has advised. Gentle activities, such as walking, can be introduced to promote healing. Be cautious to avoid any movements that strain the surgical area. Penetrative sex remains restricted during this period.
Daily Routines: You can gradually resume normal daily routines and activities that do not involve intense physical exertion. Activities like light housework or office work are generally acceptable, provided they do not cause discomfort or strain.
3. Postoperative Care and Monitoring
Follow-Up Appointments: Regular follow-up appointments with your surgeon are essential to monitor your healing progress. These visits allow your surgeon to evaluate the surgical site, address any concerns, and adjust your recovery plan as needed.
Assessment of Symptoms: Discuss any new symptoms or concerns during these appointments. Common issues might include discharge, itching, or ongoing discomfort, which can be managed by your surgeon.
4. Wound and Hygiene Care
You are expected to maintain diligent wound care as previously instructed. This includes cleaning the area with mild soap and avoiding submersion in water until cleared by your surgeon.
5. Emotional and Psychological Adjustment
As physical symptoms improve, you may still experience emotional fluctuations. This can be due to changes in body image, the impact of reduced activity, or the stress of recovery. Continue to seek emotional support from friends, family, or a mental health professional if needed. It’s important to address any feelings of frustration, anxiety, or depression that may arise during this period.
6. Healthy Habits
You are to maintain a healthy lifestyle with a balanced diet and regular, appropriate physical activity to support overall well-being and healing. Avoid smoking and excessive alcohol consumption, as these can impede the recovery process.
Long-Term Recovery: Months Two to Six After a Vaginoplasty

As you move beyond the initial recovery phase, the long-term recovery period from two to six months post-vaginoplasty involves adjusting to the changes, consolidating gains, and ensuring full functional and aesthetic outcomes. Here’s a detailed overview of what to expect and how to support your ongoing recovery during this time:
1. Functional Recovery
Final Healing Stages: By months two to six, most of the surgical site should be well-healed. However, you may still experience minor discomfort or sensitivity. This is a normal part of the final healing stages as the tissue continues to mature and integrate.
Functional Improvements: You should notice significant improvements in vaginal function, including increased tightness and enhanced sexual satisfaction. Pay attention to how the area responds to various activities and report any concerns to your healthcare provider.
2. Pelvic Floor Rehabilitation
Strengthening Exercises: Regular pelvic floor exercises, such as Kegel exercises, become increasingly important as you move into the long-term recovery phase. These exercises help strengthen the muscles around the vagina, improve support, and maintain the results of your surgery.
Physical Therapy: If recommended by your surgeon, engaging in physical therapy can further aid in strengthening the pelvic floor and addressing any residual issues or imbalances.
3. Monitoring and Follow-Up
Routine Appointments: Continue attending follow-up appointments as scheduled with your surgeon. These visits are crucial for assessing the final outcomes of the surgery, monitoring any long-term effects, and making any necessary adjustments to your recovery plan.
4. Lifestyle and Activity Adjustments
Gradual Resumption: By months two to six, you can gradually increase the intensity and duration of your physical activities. Activities like jogging, cycling, or strength training can usually be resumed with your surgeon’s approval.
Return to Sexual Activity: Sexual activity can generally be resumed by 6-8 weeks once your surgeon confirms that you are fully healed. If you experience any discomfort or changes in sexual function, discuss these with your healthcare provider.
5. Emotional and Psychological Well-Being
Mental Health and Adjustment: Adjusting to the changes in your body and the outcomes of the surgery can have emotional implications. It’s important to address any feelings of dissatisfaction or anxiety with a mental health professional if needed.
Support Networks: Continue to lean on support networks, including friends, family, or support groups. Sharing your experiences and discussing your recovery can help manage emotional challenges.
6. Long-Term Outcomes and Goals
Final Results: By the end of six months, you should be able to fully appreciate the results of your vaginoplasty. Evaluate how well the outcomes meet your initial goals and expectations.
Adjustments and Enhancements: If there are aspects of the results that are not as expected, discuss potential adjustments or enhancements with your surgeon. They can provide options for further procedures or treatments if needed.
Potential Complications Following a Vaginoplasty and How to Handle Them

While vaginoplasty is generally safe and effective, like any surgical procedure, it carries the risk of complications. Being aware of these potential issues and knowing how to manage them can help you respond promptly and effectively if they arise.
1. Infection
Signs of Infection: Look for symptoms such as increased redness, warmth, swelling, pain, or unusual discharge from the surgical site. Fever or chills can also indicate an infection.
Management
Contact Healthcare Provider: If you notice any signs of infection, contact your healthcare provider immediately. They may prescribe antibiotics or other treatments to address the infection.
Wound Care: Continue to follow strict hygiene and wound care protocols to minimize the risk of infection. Keep the area clean and dry.
2. Hematoma
Signs of Hematoma: A hematoma is a collection of blood outside the blood vessels that can cause swelling and pain. Symptoms may include localized swelling, bruising, and discomfort at the surgical site.
Management & Medical Attention: Inform your healthcare provider if you suspect a hematoma. They may perform an examination or imaging to assess the situation. Small hematomas often resolve on their own. Larger hematomas may require drainage or additional treatment to alleviate pressure and promote healing.
3. Wound Dehiscence
Signs of Wound Dehiscence: Wound dehiscence occurs when the edges of the surgical wound separate or open. Symptoms may include increased pain, a visible gap in the wound, bleeding or abnormal discharge.
Management
Seek Medical Help: Contact your healthcare provider immediately if you notice signs of wound dehiscence. They may need to perform a wound assessment and possibly re-close the wound.
Adhere to Care Instructions: Follow all wound care instructions carefully and avoid activities that could strain or disrupt the healing tissue.
4. Persistent Pain or Discomfort
Symptoms: While some discomfort is expected, persistent or severe pain that does not improve with time or medication can be a concern.
Management
Assess Underlying Causes: Persistent pain may be caused by issues such as nerve irritation or scar tissue. Your healthcare provider can evaluate and recommend appropriate interventions, such as physical therapy or pain management techniques.
Pain Management: Review your pain management plan with your healthcare provider. Adjustments to medication or additional treatments may be necessary
5. Urinary Issues
Symptoms of Urinary Complications: Issues such as difficulty urinating, pain during urination, or urinary incontinence can occur following surgery.
Management
Consult Your Provider: Report any urinary issues to your healthcare provider. They can assess for possible complications like urethral stricture or other post-surgical effects.
6. Sexual Dysfunction
Symptoms: Difficulties with sexual function, such as pain during intercourse, reduced sensation, or problems achieving orgasm, can be experienced post-surgery.
Management
Open Communication: Discuss any sexual concerns with your healthcare provider. They can offer guidance on addressing these issues, including potential treatments or adjustments to your recovery plan.
Sexual Therapy: Consider speaking with a sexual health therapist or counsellor if needed. They can provide strategies and support for overcoming sexual dysfunction and enhancing sexual satisfaction.
7. Scarring and Aesthetic Concerns
Visible Scarring: Scarring or changes in the appearance of the surgical site may occur. This can include keloids or hypertrophic scars.
Management
Follow-Up Care: Regular follow-up appointments with your surgeon can help monitor and address any scarring concerns. They may recommend treatments like silicone gel sheeting or laser therapy to improve the appearance of scars.
By being proactive and informed about these potential complications, you can better manage your recovery and address issues promptly. Always consult with your healthcare provider if you have any concerns or symptoms that deviate from your expected recovery path.
When to Seek Medical Attention
Seek medical attention after a vaginoplasty if you experience any signs of infection, such as increased redness, swelling, warmth, or unusual discharge accompanied by fever or chills. Immediate attention is also required if you notice significant pain that worsens despite medication, if you have trouble urinating, or if the surgical site shows any signs of separation or opening.

Persistent discomfort during sexual activity, significant changes in sensation, or any unusual symptoms should also prompt a consultation with your healthcare provider. Promptly addressing these issues can help prevent complications and ensure a smoother recovery.
Proper Recovery With Professional Care
Recovering from vaginoplasty is a gradual process that extends over several months. Understanding each stage, from managing initial pain to resuming normal activities and addressing complications, enhances healing.

Following your surgeon’s instructions, maintaining hygiene, and caring for your physical and emotional well-being are key to a successful outcome. At Labiaplasty NYC, we perform all procedures with proper care and with our regular follow-up appointments, you can expect improved function, confidence, and overall quality of life. Book an appointment today to speak with one of our gynecological experts.
References
- Green FJ. From clitoridectomies to ‘designer vaginas’: The medical construction of heteronormative female bodies and sexuality through female genital cutting. Sexualities, Evolution & Gender. 2005 Aug 1;7(2):153-87.
- Goodman MP. Female genital cosmetic and plastic surgery: a review J Sex Med. 2011; 8:1813–1825.
- Jamali S, Abedi P, Rasekh A, Mohammadjafari R. The long term effect of elective colpoperineoplasty on sexual function in the reproductive aged women in Iran. International scholarly research notices. 2014;2014(1):912786.
- Furnas HJ, Canales FL. Vaginoplasty and perineoplasty. Plastic and Reconstructive Surgery–Global Open. 2017 Nov 1;5(11):e1558.
- Qureshi AA, Tenenbaum MM, Myckatyn TM. Nonsurgical vulvovaginal rejuvenation with radiofrequency and laser devices: a literature review and comprehensive update for aesthetic surgeons. Aesthetic surgery journal. 2018 Feb 15;38(3):302-11.